
What is the purpose of a hysteroscopy
What is the purpose of a hysteroscopy?
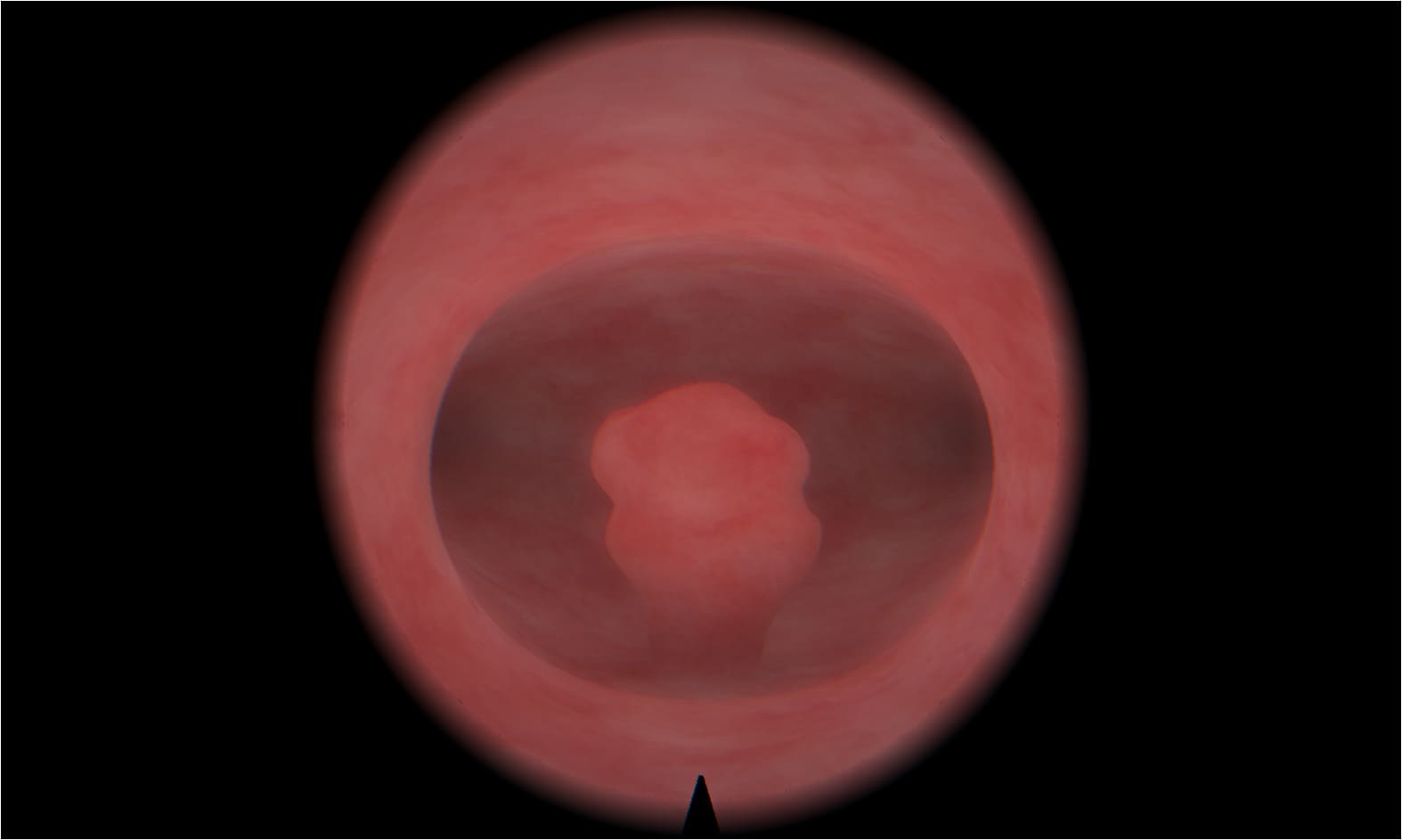
Hysteroscopy is a non-invasive medical procedure that allows a clinician to examine the inside of the uterus using a thin, lighted instrument known as a hysteroscope. This method is employed both diagnostically and therapeutically to investigate abnormal uterine conditions such as heavy menstrual bleeding, infertility, or recurrent miscarriage. The visual clarity provided by hysteroscopy supports precise interventions and reduces the need for more invasive surgeries.
Why is hysteroscopy performed?
The primary purpose of a hysteroscopy is to identify and often treat intrauterine abnormalities. This may include removing polyps or fibroids, assessing uterine adhesions, correcting congenital anomalies, or investigating causes of abnormal bleeding. The hysteroscope gives direct visual access to the uterine cavity, making the procedure more accurate than blind dilation and curettage (D&C).
Some common conditions evaluated or treated via hysteroscopy include:
- Endometrial polyps
- Submucosal fibroids
- Intrauterine adhesions (Asherman’s syndrome)
- Congenital uterine septum
- Retained products of conception
How is hysteroscopy carried out?
A hysteroscopy typically takes place in a clinical or hospital setting, and depending on its purpose, may be performed under local, regional, or general anesthesia. The hysteroscope is gently inserted through the cervix into the uterus, where a saline solution or carbon dioxide is introduced to expand the cavity for enhanced visibility. This allows the practitioner to examine or treat the uterine lining without incisions or prolonged recovery time.
Is hysteroscopy painful or risky?
While hysteroscopy is generally considered safe and well-tolerated, individual experiences vary. Diagnostic procedures, particularly those without anesthesia, may cause mild cramping or discomfort similar to menstrual pain. Therapeutic hysteroscopy, involving the removal of fibroids or adhesions, may require sedation or anesthesia to minimize pain.
The risks associated with hysteroscopy are rare but can include:
- Infection of the uterus
- Uterine perforation
- Cervical injury
- Fluid overload (especially in lengthy procedures)
Despite these minimal risks, hysteroscopy remains a preferred option due to its direct visualization, precision, and low complication rates.
What are the benefits of hysteroscopy compared to traditional methods?
Unlike traditional procedures such as blind curettage or exploratory laparotomy, hysteroscopy offers superior visibility, real-time decision-making, and minimally invasive access to the uterine environment. This translates into:
- Faster recovery times
- Reduced need for hospitalization
- Minimized postoperative pain
- Lower risk of surgical complications
- Enhanced diagnostic accuracy
These advantages make hysteroscopy an invaluable tool in modern gynecology, particularly when managing unexplained infertility or abnormal uterine bleeding.
When is hysteroscopy recommended?
Clinicians often recommend hysteroscopy in the following scenarios:
- Persistent or heavy menstrual bleeding
- Recurrent pregnancy loss
- Unexplained infertility
- Abnormal findings on ultrasound
- Postmenopausal bleeding
- Suspected endometrial hyperplasia or cancer
In each of these cases, hysteroscopy serves as both a diagnostic and therapeutic modality, enabling precise intervention without resorting to open surgery.
Can hysteroscopy aid fertility treatment?
Yes, hysteroscopy plays a critical role in evaluating and enhancing female fertility. It enables clinicians to detect and address anatomical anomalies within the uterus that might hinder implantation or increase the likelihood of miscarriage. By removing polyps, fibroids, or adhesions, the uterine cavity is restored to an optimal state for conception, whether naturally or via assisted reproductive technologies.
For patients undergoing IVF or intrauterine insemination (IUI), a prior hysteroscopy may significantly increase success rates by ensuring the endometrial environment is conducive to embryo implantation. This makes it an essential step in many fertility clinics’ diagnostic protocols.
What’s the difference between diagnostic and operative hysteroscopy?
There are two principal types of hysteroscopy: diagnostic and operative.
- Diagnostic hysteroscopy is used solely to observe the uterine cavity and identify abnormalities. It is often done in an outpatient setting and requires minimal anesthesia.
- Operative hysteroscopy is conducted to correct structural issues, often during the same session. This involves inserting surgical instruments through the hysteroscope to perform tasks such as polyp removal or septum resection.
The ability to seamlessly transition from diagnosis to treatment in one sitting is one of hysteroscopy’s greatest clinical advantages.

How should one prepare for a hysteroscopy?
Preparation for hysteroscopy depends on the nature of the procedure. Patients may be advised to:
- Avoid intercourse a few days prior
- Cease certain medications
- Schedule the procedure during the early phase of the menstrual cycle
- Fast for several hours if general anesthesia is planned
Pre-procedural counseling also covers risks, benefits, and post-procedure care, ensuring informed consent and reducing patient anxiety.
Q&A
Can hysteroscopy detect cancer?
Yes. Hysteroscopy allows direct visualization and biopsy of suspicious areas within the uterus, making it a vital tool in the early detection of endometrial cancer.
Does hysteroscopy affect future menstrual cycles?
It might. Many patients report lighter, more regular periods after the removal of polyps or fibroids. However, each case is unique and outcomes vary.
How long does recovery take after hysteroscopy?
Recovery time is typically short. Most individuals return to normal activities within 24–48 hours, although some may experience mild cramping or spotting for a few days.
Can you get pregnant after a hysteroscopy?
Yes. In fact, for many women, hysteroscopy is a step toward improving fertility. By correcting structural abnormalities, it enhances the chances of conception either naturally or via assisted reproductive methods.
Is anesthesia required for hysteroscopy?
Not always. Diagnostic hysteroscopy is often performed without anesthesia, though mild sedation or local anesthesia may be used to increase comfort. Operative procedures usually require general or regional anesthesia.
Immerse yourself in a demo to see how MedVision transforms traditional learning into an engaging, interactive experience
Subscribe for the Latest News!





